A diagnosis of triple negative breast cancer (TNBC) means that the three most common types of receptors known to fuel most breast cancer growth–estrogen, progesterone, and the hormone epiderm al growth factor receptor 2 (HER-2) gene– are not present in the tumor. Since these receptors are not present, common treatments like hormone therapy and drugs that target estrogen, progesterone, and HER-2 are ineffective and therefore make the cancer more challenging to treat. However, other medicines and combinations of surgery, radiation therapy, and chemotherapy have been used to successfully treat TNBC. TNBC can have the same symptoms and warning signs as other types of breast cancers, and it represents 10-15% of all breast cancers. TNBC has shown to be more prevalent in:
- Premenopausal African-American women
- Women with an elevated hip-to-waist ratio
- Women who have had fewer children
- Women who have not breastfed, or breastfed for shorter lengths of time
- Younger women, under the age of 40 or 50
- Those with the BRCA1/BRCA2 gene mutations
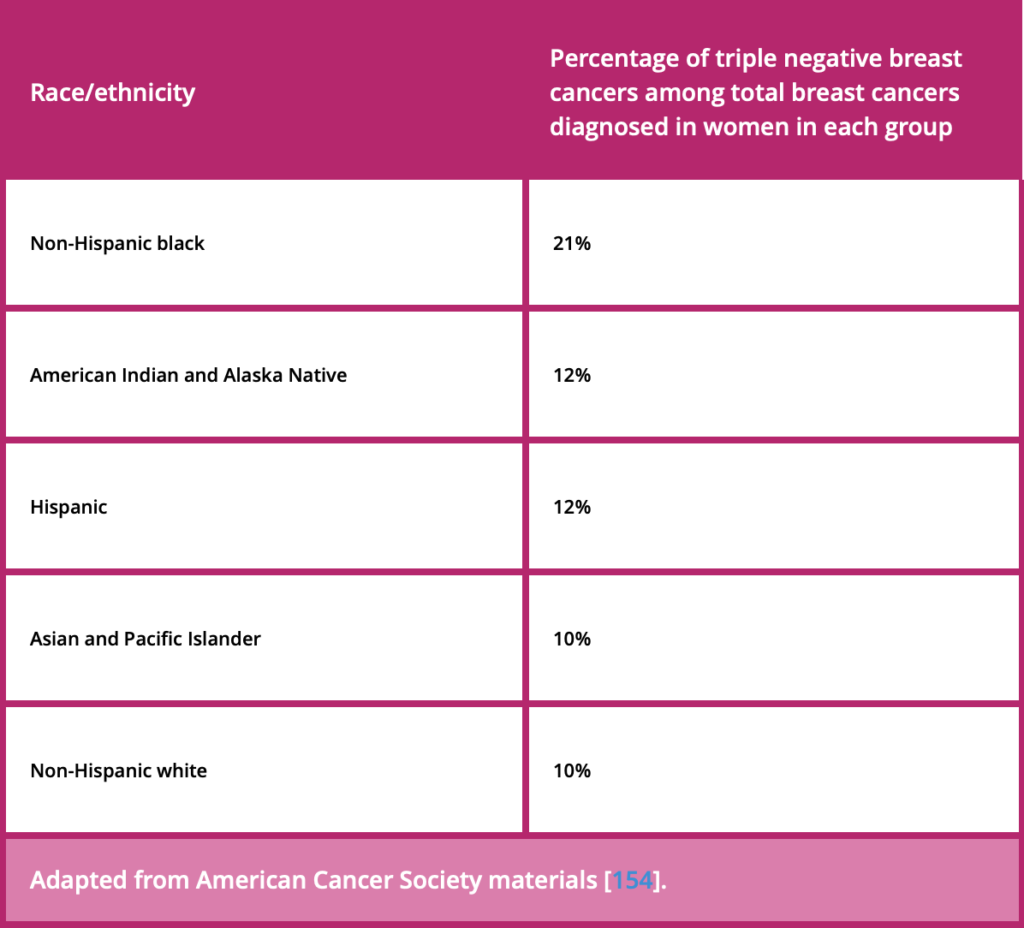
Triple-negative breast cancer occurs at different rates among races and ethnicities. Although the reasons for these differences is unclear, TNBC is more frequent among non-Hispanic black women diagnosed with breast cancer, than non-Hispanic white women diagnosed with breast cancer.
Because TNBC cells lack estrogen and progesterone receptors and do not overexpress the HER2 gene, the cancer cells do not respond to hormone therapy or medications that block HER2 receptors. Instead, TNBC treatment involves chemotherapy, radiation, and surgery (either a lumpectomy or mastectomy). Studies show that triple negative breast cancer may respond even better to chemotherapy in earlier stages than other forms hormone receptor-positive breast cancers. The standard care for triple-negative is chemotherapy before surgery. Recently, the addition of newer medications called poly ADP-ribose polymerase (PARP) inhibitors, and other immunotherapies, have shown to be promising treatments for TNBC. Different subtypes of TNBC each have unique abnormalities, which can serve as targets for treatment drugs. Ongoing clinical research is being conducted to improve current and future treatments. After treatment, be sure to continue with a regular appointment schedule. It is important to take charge of your health by maintaining a good diet and exercising. Meditation, support groups, or therapy also offer positive emotional balance.
TNBC is considered an aggressive cancer, as it grows at a quicker rate, is more likely to have spread upon diagnosis, and has a higher chance of coming back after treatment than other forms of breast cancer. 5-year survival rates for TNBC are shown in the chart below, based on women diagnosed with triple-negative breast cancer between 2010 and 2015. This data is courtesy of the American Cancer Society, which relies on data from the National Cancer Institute’s SEER database. SEER tracks 5-year relative survival rates for breast cancer in the United States based on how far the cancer has spread. It does not group cancers by stages (stage 1, stage 2, etc.), but instead groups cancers into three categories:
- Localized: No sign that the cancer has spread outside the breast.
- Regional: Cancer has spread outside the breast to nearby structures or lymph nodes.
- Distant: Cancer has spread to distant parts of the body, such as lungs, liver, or bones.
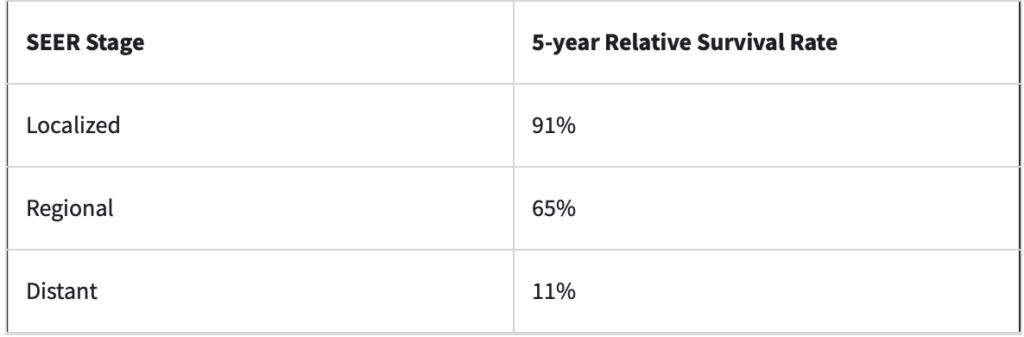
Remember that every individual has a unique experience with the disease that cannot be exclusively defined by statistics. Survival rates are estimates based on previous outcomes. No one can exactly predict how your breast cancer will progress or respond to treatment. Women being diagnosed right now may have a better outlook than these numbers show, as treatments improve over time. These numbers only apply to the stage of the cancer when first diagnosed and do not take into consideration cancer growth, spread, or return. It is also important to note that while TNBC is more likely to return within five years than other forms of breast cancer, it rarely relapses after that first five-year period, which offers patients a confident feeling of beating their cancer. Each individuals’ case and experience with cancer is unique. Consult your doctor about how these numbers apply to you and how you can reduce your risk of recurrence.
Click here for a video by the National Breast Cancer Foundation that helps explain the basics of TNBC.
Resources
Godman, Heidi. “Triple Negative Breast Cancer Outlook: Survival Rates.” healthline, December 9, 2019. https://www.healthline.com/health/triple-negative-breast-cancer-outlook-survival-rates-stage.
Nathan-Garner, Laura, and MD Anderson Cancer Center. “Triple-Negative Breast Cancer: 5 Things You Should Know,” April 30, 2015. https://www.mdanderson.org/publications/cancerwise/triple-negative-breast-cancer-5-things-you-should-know.h00-158986656.html.
Silberman, Ann. “Recurrence Rate for Triple-Negative Breast Cancer.” healthline, October 8, 2018. https://www.healthline.com/health/triple-negative-breast-cancer-recurrence.
“Triple Negative Breast Cancer.” National Breast Cancer Foundation. Accessed June 2, 2020. https://www.nationalbreastcancer.org/triple-negative-breast-cancer.
“Triple Negative Breast Cancer.” Susan G. Komen®, May 21, 2020. https://ww5.komen.org/BreastCancer/TripleNegativeBreastCancer.html.
“Triple-Negative Breast Cancer.” Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, July 26, 2019. https://www.cdc.gov/cancer/breast/triple-negative.htm.
“Triple-Negative Breast Cancer: Details, Diagnosis, and Signs.” American Cancer Society, September 20, 2019. https://www.cancer.org/cancer/breast-cancer/understanding-a-breast-cancer-diagnosis/types-of-breast-cancer/triple-negative.html.
“Triple-Negative Breast Cancer: Overview, Treatment, and More.” Breastcancer.org, May 13, 2020. https://www.breastcancer.org/symptoms/diagnosis/trip_neg.